Telehealth Toolkit
PROVIDING EXCELLENT SERVICES
VIA VIRTUAL PLATFORM
Victor Community Support Services
& Treatment Centers, inc.
©2021 Victor. All Rights Reserved.
Acknowledgements
Authors and Contributors
Hannah Buerger
Coral Boyle-Day, Associate MFT
Beau Compau, LCSW
Giana Kooger, LMFT
Andrea Lovvorn, LCSW
Kaitlyn Marsh, LMFT
Sophia McKean
Edgar Melendez, Associate MFT
Joseph Olvera, LMFT
Amy Rudkin, LCSW
Emily Seagraves, LCSW
Jackie Seefeldt, LMFT
Table of Contents
What do we mean when we say "telehealth"?
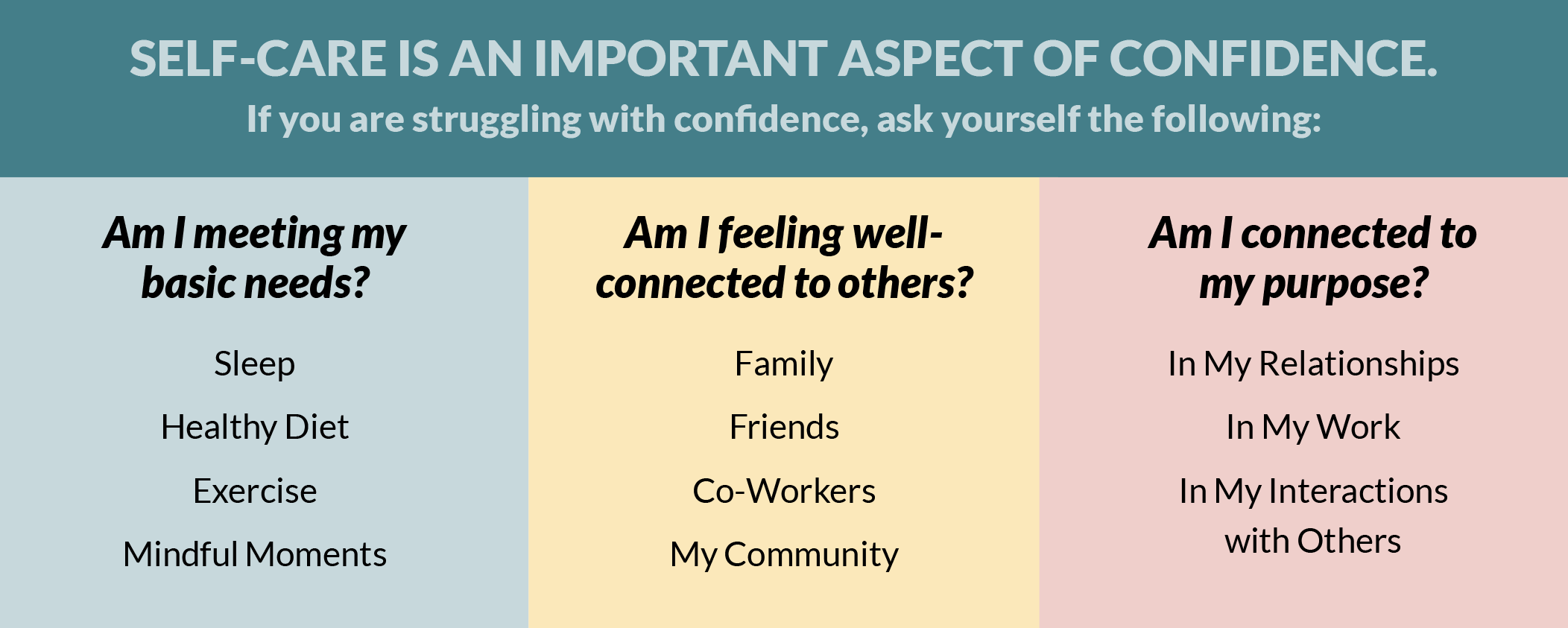
But what if I don't feel confident?
Confidentiality and the Therapeutic Environment
Come Prepared: Have a Plan and a Back-Up Plan
Making the Most of Zoom as a Virtual Platform
Elementary and Middle School Aged Population
Assessing and Addressing Crisis Virtually
Victor CQI: Telehealth Procedural Guidelines
Informed Consent for Telehealth (example)
Introduction
Since the onset of COVID-19 in California in March 2020, mental health service delivery at Victor has transformed drastically in order to best protect the physical health of staff, clients, and the general public.
For most, this has looked like a shift from a community- or office-based model to one that primarily relies on telehealth to meet the complex needs of the clients and families that we serve. While telehealth services have always had a place in the mental health world, this abrupt and unplanned shift away from our standard service model left many suddenly wondering how they would continue to access the skills and tools necessary to feel successful in their work. Many had to re-write their playbook entirely. This shift has required significant adaptability at every level of the organization, but has been felt most profoundly by those working directly with youth and their families.
We have found over the last year that Victor staff have remained true to Victor's core values of teamwork, excellence, adaptability, and mission-driven and have faced this challenge with persistence and creativity.
As an agency, we now have the knowledge and skillset required to confidently add "telehealth" to the wide array of service delivery options that we provide with excellence. At times, we have even found that telehealth has been a preferred method of service delivery that has given us the opportunity to access and serve clients in ways that in-person services would not have allowed for. This document is intended to serve as a resource for those wishing to understand more about how to provide excellent services on a telehealth platform.
What do we mean when we say "telehealth"?
Telehealth services are any client-related services (assessment, treatment planning, therapeutic and rehabilitation services, collateral support, groups, Child and Family Team meetings) that are provided via virtual platform or telephone.
It is important to note that telehealth is not a type of therapy itself, but rather a mechanism to deliver mental health services.
Many different evidence-based therapeutic practices can be successfully translated to be delivered via telehealth. Please note that this document assumes a baseline of knowledge in Victor's general practices as well as best practice approaches for the client populations that we serve. This document will discuss how strategies and interventions previously tailored to in-person services can be translated into virtual work; however, it will not go into significant detail about standards of practice for in-person services.
Laying the Groundwork
When understanding what is required to perform telehealth work with success, keep in mind the "Three C's": Confidence, Containment, and Competence. These 3 areas of focus will provide the framework for the rest of this toolkit.
Confidence lays the foundation of successful telehealth work. Do you believe in your ability to provide excellent care virtually, and can you help your clients believe it will be effective too?
Containment refers to the aspects of care that you need to consider in order to create and maintain a safe therapeutic space for your clients.
Competence provides you with tools and considerations for delivering telehealth services with excellence. The bulk of this toolkit focuses on competence across various client populations and service types (age 0-5, elementary and middle school-aged children, Transitional Aged Youth, group work, CFT Meetings, and crisis response).
Confidence
How you present yourself in a virtual setting is extremely important.
Clients and their families want to be held and led by someone who can convey an authoritative air (that is, a presence that conveys high expectations coupled with high warmth). It is up to you to take charge of the virtual room and be directive with all participants to keep the session focused, on track, and productive. It is critical that you present as someone who is assured that effective work can be done via telehealth, and that you have the tools to guide the client there.
Educating yourself on the aspects of containment and competence detailed in the rest of this toolkit is an important first step in increasing your confidence.
Be clear and realistic in your goals for yourself, your clients, and your sessions. Telehealth services will not perfectly replicate in-person support, and that's OK. Services might be shorter, "success" might be measured differently, and the strategies you employ will certainly be different. It is important to know what you are aiming to achieve and to create a shared understanding of these goals with your clients and families.
Please note that when comparing telehealth and in-person services, we are emphasizing that telehealth services are different than in-person services, not that they are less effective.
It is true that certain clients and certain populations might require or get more benefit from in-person support; part of your work is to continuously analyze service effectiveness in comparison to risk factors with your supervisor to ensure that you are appropriately meeting the needs of any given client.
We have found, however, that for a large portion of our client population, clients and their families are able to adapt well to a telehealth model and make progress when the right strategies are put in place. In fact, at times, we have found increased benefits from telehealth support, many of which we will discuss throughout this toolkit.
But what if I don't feel confident?
It is important to be honest and realistic but not negative about telehealth service delivery.
If you begin a telehealth relationship by underselling your ability to make a significant impact on a virtual platform, families will immediately begin to hold doubt about the ability of your services to be effective. It is perfectly natural that you as a service provider might experience feelings of insecurity or even doubt your own effectiveness to provide services virtually. This is new territory for most workers in the mental health field. If you find yourself experiencing these types of feelings, it is important to talk with your supervisor and understand how to work past this.
Entering a new therapeutic relationship with confidence and authority (even if you have to fake it at first) will make a huge impact in a client's ability and desire to stick with you through this.
Know what you expect from clients related to engagement and hold these expectations with authority. However, you should also remain open to clients' feelings and experiences related to services looking "different" than they might have pictured as well. Through doing this work personally, hopefully you can find appropriate moments to join with clients in their uncertainty and share with them how you managed to work through your own skepticism and anxiety and what you've learned along the way.
Containment
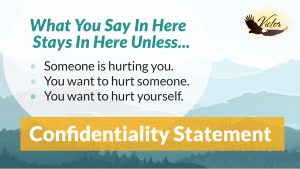
Confidentiality and the Therapeutic Environment
When beginning telehealth work with a new client, keep in mind that receiving virtual mental health care may be a new experience for them. It is up to you as the service provider to clearly create and maintain the boundaries that will be required for this work to be done successfully. Clients will be looking to you to lay out what they can expect from your service, and to help create the environment in which that service can do its intended purpose. If deviations occur throughout the course of services, it is up to you to help create the plan that will bring things back on track.
- Be informed of Victor’s specific guidelines and regulations related to privacy and telehealth services. Have a discussion with your supervisor about your site’s practices, and refer to the “Victor CQI: Telehealth Procedural Guidelines” in the appendix of this toolkit.
- Create a secure work environment for yourself that respects the privacy and confidentiality of your clients
- Consider who the other people are in your home/workspace when working remotely and take appropriate precautions to ensure that they will not overhear your sessions or interrupt while you are meeting with clients
- Treat your session time as sacred: ensure that you are 100% focused on your client during your session and not navigating outside distractions
- Try to be in the same environment each time you meet with your client; this will create a sense of routine and predictability for your time together
- For additional telehealth assessment questions that you may want to explore to better understand your telehealth environment needs, see the “Telehealth Needs Assessment (West Coast Children’s Clinic)” in the appendix.
- Assist clients and their families in creating a consistent therapeutic environment on their end as well
- Brainstorm barriers to confidentiality (no private space in home, interruptions from family members) and assist client in identifying solutions to these barriers
- Be clear in your expectation of how session time will be honored. If you prefer that clients meet with their screens on, provide undivided attention, or not engage in other distracting tasks while meeting, you must say so and explore reasons why clients might feel challenged to uphold these expectations
- Create agreements during your first session about ways in which you will both respect one another’s time; this way, if behaviors have to be challenged in the future, you can fall back on the shared agreements already created
- Provide clients and families with a “telehealth overview” that tells them what to expect from services – what services are as well as what services are not. See the “Telehealth Informed Consent” in the appendix of this toolkit to help guide this discussion as well.
- Lay the ground work at the beginning of each session about what client can expect –what you will do for your meeting and how long you intend to meet for. This can help keep clients focused and away from distractions.
Come Prepared:
Have a Plan and a Back-Up Plan
No matter what method of service delivery you are employing, you will find the most successful engagement if clients and families can trust your ability to do what you are setting out to do.
This is especially true in telehealth; when providing in-person services, a lack of preparedness can sometimes be masked by transitioning to relationally-oriented conversation or using non-verbal cues to build warmth and rapport. In telehealth, these types of strategies are largely unavailable.
Clients’ perceptions of your abilities to create a safe container will be a primary selling point in their willingness to continue meeting with you.
Some strategies to create emotional
containment virtually:
- PLAN AHEAD. Always enter sessions with a clearly thought out objective and agenda. Even if your objective is loose and non-specific, knowing what you intend to do with your time will help create structure.
- Come prepared with an intervention to increase participation and engagement. Root yourself in how your chosen interventions speak to client’s larger goals.
- Have a back-up plan in case the client does not want to do your planned activity.
- Know ahead of time how you intend to respond if the client is non-participative, is feeling highly emotional, or is in crisis (see section titled “Assessing and Addressing Crisis Virtually” for more information)
- Know your technology; understand how to navigate your chosen platform and have a back-up plan of how you will respond if either you or your client experience technical difficulties
Making the Most of Zoom as a Virtual Platform
Zoom is Victor’s preferred platform for providing telehealth services. The platform has a wide array of features that can provide opportunities to make sessions more interactive, increase engagement, and add creative touches that would not be available to capitalize on during in-person sessions. Knowing the ins and outs of your technology as well as being prepared to troubleshoot any challenges will increase clients’ overall sense of your ability to manage and contain the space.
The Basics of Zoom
Below are links to tutorials that will help you learn about various functions and controls on this platform.
- Basic Zoom Controls (10:17)
- Top 20 Zoom Tips and Tricks (20:10)
- New Zoom features (note that some overlap with Top 20 Tips and Tricks) (15:53)
You can also visit Zoom’s official support page for specific troubleshooting needs
Intervention-Friendly Features
Zoom also has a wide array of features that can be utilized to increase participation and engagement in sessions. Below are some features to be aware of; however this list is not exhaustive. You are highly encouraged to do your own research as well depending on your or your clients’ specific needs.
- Shortcut Keys (Settings-Keyboard Shortcuts)
- There are many shortcut keys you can use and/or customize for easy navigation. For example, when muted, press and hold spacebar to temporarily unmute while you make a quick comment.
- Share Screen Options
- The Whiteboard option can be used for interactive individual or group sessions (Pictionary, Tic-Tac-Toe, Hangman, Illustrating Psychoeducation, etc.)
- Multiple screens can be shared by the host and also by different participants (host can control if participants are allowed to share screen). To share multiple screens, press the control key when selecting screens to share.
- When showing a PowerPoint, you can have the PowerPoint as the background with your image showing. You can move your image and also change the size of your image so that content is not blocked.
- Annotation allows participants to write or draw on the host’s screen share. This can be utilized to sign non-legal documents such as a safety agreement or engagement contract, or to increase client’s buy-in as well as attention to detail.
- Backgrounds and Filters
- Backgrounds can be used for themes or privacy. Consider using a background for your own personal privacy if you are providing a session from your home.
- When using a background, click the box “I have a green screen”. This adds detail to your image so you don’t look as cut and pasted onto the background and improves the filtering between you and the background.
- Video Filters can add fun and increase interaction in a session. For example, clients can make themselves a bunny or add a chef hat (plus many more options to explore!).
- Upload custom images for backgrounds to simulate therapy rooms. This can be utilized to create routine environments for clients or ability to “walk” into different rooms/spaces to differentiate between intervention and gameplay.
- Audio Features (Settings-Audio)
- You can Suppress Background Noise (auto, low, medium, high)
- You can click to join by computer audio automatically when opening a meeting
- You can click “mute when joining” so you are sure background noises are eliminated
- Cultural inclusion: You can change your thumbs up reaction skin tone
- Closed Captioning is possible for hearing impaired clients. Here is a link for instructions on this feature: View Closed Captioning.
- Breakout Groups
- You can make a participant a co-host and they will be able to help you manage breakout groups
- You can select breakout group participants when scheduling the meeting. During the meeting when you start the breakout groups, have Zoom randomly distribute the people into groups, or allow the participants to choose their own group
- Video Features (Settings-Video)
- You can touch up your image
- You can improve appearance when there is low light
- Hide/Show Self-View: Encourage participants to hide self-view so that their camera remains on however not visible to them. This can reduce distractions as well as decrease self-consciousness.
Competence
The rest of this toolkit will focus on competence, detailing strategies to increase engagement and address common barriers that arise when providing telehealth services. Sections have been broken down by age group of the client being served: early childhood, elementary & middle school aged, and Transitional Age Youth. They are followed by additional categories to address specific service types: groups, CFT Meetings, and crisis response. These categories have been identified to address the many differences that arise in attempting to best serve these unique populations, however you will find that some of these strategies translate across age categories as well.
Early Childhood (0-5 years)
Young children can present with unique challenges when it comes to virtual engagement, as so much therapeutic rapport is usually created through physically interactive activities, play, and body language. When engaging a young child in a telehealth session, be attuned to their specific developmental abilities and tailor your approach to be entertaining, high energy, and visually interesting (this may require an extra cup of coffee before a session!).
In addition, for children who are 0-5, caregiver involvement is crucial to the effectiveness of services. Caregiver involvement is always important for children this age, as many of the therapeutic interventions will happen through or with the support of the caregiver. When providing these services via telehealth, constant involvement or supervision from the caregiver is recommended. This is a big change from office-based services in which caregivers can drop their child off at a therapy session and have a free hour. It will be important to assess caregivers’ willingness and ability to participate actively in the child’s therapeutic process, and help troubleshoot barriers to their involvement. You should expect that when providing telehealth services to young children, even more of your therapeutic time than usual will be dedicated to collateral support of their caregiver and plan for this accordingly in your schedule.
Getting Started and Building Engagement
With the Caregiver:
Many of the caregivers we work with may not have capacity for this high level of involvement during sessions. Other caregivers may have unrealistic expectations of their child’s development and ability to manage sessions independently via virtual platform.
During the initial appointment, discuss the expectations of the caregiver, which should include a conversation on follow through on activities and assignments between sessions.
Ask questions and hear caregivers out about their self-assessed ability to participate as requested.
Some factors to discuss early in treatment:
- Speak with the caregiver about “prepping” the child for each session by reminding them of the appointment, helping them get excited or motivated to participate, and giving the child clear directives about what is expected
- Request that the caregiver remain nearby during sessions to help redirect the child if they lose focus or maintain safety if they become upset
- Alternatively, create a plan for how the child can be given “space” in the home when needed, if sensitive therapeutic subjects might be explored
- Discuss play materials and props that could be used by the child during your sessions. Explore what items the caregiver already has in the home that could be utilized. If there are additional materials you’d like the child to have access to, consider purchasing them (as your program allows) to be kept at the family’s home. Request that the caregiver only allow use of purchased items during therapy sessions. Some recommended items include: paper and pen/markers/crayons, toys or stuffed animals, sensory toy(s), Play-Doh, squishies, clay, fidget toys, or any comforting item that may have special meaning to an individual child
- Discuss any “rules” that the caregiver has about their home so that you can help create shared boundaries. Honor these boundaries throughout the therapeutic relationship
- Assessment for a young child will require quite a bit of in-vivo observation of their interactions with their caregiver. Consider the types of activities that you would engage a child in in-person when conducting an initial assessment. Coach the caregiver in what you are looking for, and how you would like them to respond to the child in these moments; treat them as a co-facilitator of the session to help empower them
With the Child:
When engaging a young child via telehealth, you will find the most success if you MAKE IT FUN! In this platform you are as much a performer as you are a therapist. Keep your tone energized, provide the child with 100% of your attention, and allow as much space as possible for creativity. There are a multitude of resources online that provide ideas for activities and interventions with this population, some of which we will list at the end of this section. Here are some suggested strategies and considerations to get the ball rolling as you engage with a new child:
- Develop a consistent “therapy space” through the introduction of a grounding practice or ritual at the beginning of each session. Young children thrive on routine and predictability – think Mr. Rogers!
- Know who else is present in the home. Be mindful of other family members being present when asking questions about history, symptoms, and behaviors as these may be triggering or upsetting if others are unprepared
- Have an arsenal of silly costumes (hats, wigs, glasses) that you can put on to bring levity as needed
- Make use of the child’s toys already present in their home. This can be helpful if they feel particularly attached to a stuffed animal, for example. Think of ways to introduce their prized possessions into session. This can be especially useful during assessment. Consider “interviewing” a child’s stuffed animals by asking questions that you’d like to know about the child
- Make it fun! Engage the caregiver proactively in the session with the child and suggest “out of the box” activities such as nature walks, zoom calls with friends, board games, sharing of family stories, puzzles, or a family baking activity
- Art-based activities are a great option for this population. One such activity: have the child draw a house. Who lives there? What goes on inside? What’s it like at night? Do people visit there?
- Help keep the child focused and calm. Have a list of “settle strategies” to utilize when the child needs to be re-grounded during a session. Here is a non-exhaustive list:
- Take deep breaths
- Get a hug
- Draw or color
- Eat a snack
- Take a rest
- Do a silly dance
- Count to 10 super fast, then super slow, then super fast, then super slow
- Do animal breaths (butterfly, elephant, bee, dog, horse, etc.)
- Sing a song
- Say your ABC’s
- Hug a favorite toy or do breaths together with your toy
- Scream into a pillow
- Jump up and down
- Listen to music
- Dance like crazy to your favorite song (pull up that song and have a dance right in the moment)
- Squish something soft
- Watch the clouds
- Stomp feet
- Shake parts of or whole body
- Tear up paper
- Pop bubble wrap bubbles
Links to Additional Interventions and Resources:
Sesame Street in Communities: includes trainings as well as free printables and activities that can be used in session with young children
Online Sand Tray: share your screen and bring sand tray therapy to the virtual world
Teletherapy Activities: 50 teletherapy ideas to use with young children
Ages and Stages: Provides a link to Ages and Stages Questionnaire (ASQ-3) interventions that you can coach parents to use oruse in session yourself. Interventions are broken out by age
Intervention Activities for young children: 20 more interventions ideas to use with young children
Prevention: Prevention Works Video Library
Additional Intervention Tools: Additional intervention ideas for children and youth
Elementary and Middle School Aged Population
In comparison to their older or younger counterparts, there are interesting benefits and challenges to providing telehealth services to clients who fall “in the middle” age range of those we serve. Unlike younger children, they are often developmentally able to engage in a session with more independence (although please keep in mind that it is important to assess the developmental age of your clients, and for clients who present younger than their actual age, it may be wise to employ interventions specific to younger children). However, they may not be quite as engaged in talk-based therapy or as “bought in” to services as their older counterparts either. Working with this age range requires a unique blend of appealing to clients’ autonomy and increasing maturity, while also creating an environment that is fun and stimulating to maintain their interest.
Challenges to Consider and Potential Solutions
Privacy
Unlike with younger children, it will likely be less effective and appropriate to have a caregiver in the immediate vicinity or actively participating during entire sessions.
Consistent collateral engagement remains appropriate with this population, however it is also increasingly important that clients have their own “private” space to explore their feelings and engage with you. Consider discussing with the youth and caregiver during initial sessions:
- What are the shared expectations for privacy during sessions and how can that be achieved? Caregivers may need to be prompted to help create a quiet, secluded space where the youth feels secure.
- In the event that homes don’t allow for complete privacy (too many family members around, no private areas), discuss the potential impact with the youth and their caregiver. It may require altering your strategies and approach; for example, focusing on behavior-based interventions rather than talk-based processing, or conducting sessions as family sessions.
- Discuss how the caregiver will still be involved in keeping the youth focused and engaged in sessions. Create a plan for how you will notify the caregiver if you need their assistance re-focusing the youth during a session.
Promoting Increased Autonomy
Clients at this age do not want to be “babied” and will respond to your attempts to help them exert independence and control over your time together. Some ways to promote this via telehealth:
- Be open to allowing the client to drive the length of the session. Either establish this with them ahead of time (“would you like to meet for 30 minutes or 40 minutes today?”) or read the room and be open to shortening a session if they are struggling or disengaged. Plan that your sessions in general might be shorter than when meeting in-person.
- Provide clients with a list of options of activities for any given session.
- Be as open as appropriate with clients about your process (“I’m asking you this question because…”) as a means to increase verbal engagement and normalize the “talking” aspect of your relationship.
- For clients who are familiar with in-person therapy, have an open discussion about what might be “different” versus “the same” in telehealth. Ask clients what they might feel nervous or unsure about in telehealth. Revisit this topic frequently throughout the therapeutic relationship.
Creating an Engaging Space
In addition to promoting autonomy and honoring maturity, you will also want to be sure to create a setting that feels fun, engaging, and contained for clients to maximize their experience. Some strategies and resources to consider:
- Utilize Google to create a virtual “therapy room” for your sessions. This is a great way to keep kids interested, and you can use this as a launching pad for other interactive activities. See the following YouTube tutorials (created by a member of the Victor team) for this step-by-step process:
- Create your Google account (ensure that you create a new account with your Victor information as opposed to linking this to your personal Google account) (2:07): Creating a Google account
- Create a Bitmoji account and add the Google extension (5:39):
- Finally, create the virtual therapy room (16:51):
- Use the Whiteboard function in Zoom to draw pictures together with your client virtually.
- Upload therapeutic workbooks to your computer so that you can screen share them with your client and go through them together interactively. Alternatively, you could drop off physical workbooks ahead of time at clients’ homes.
- Consider fun, hands-on activities that you can facilitate safely remotely. Engage the client in a cooking or baking project, drop off art supplies for a specific art project, or have them do a “show and tell” of special items in their home and discuss their meaning.
- Web-based games are a great option for this population. Here are links to a few options and ideas:
- Create Avatars online (have clients create representatives of themselves and important people in their lives)
- Do jigsaw puzzles together
- Play Connect Four or other traditional board games:
- Feelings-based Mad Libs
- 2-Player Online Games
- View this YouTube video detailing games and activities to play via Zoom
- Do a virtual Escape Room! This link also has walkthrough videos in the event you get stuck (highly recommended to view those before your session):
- Emotions Scavenger Hunt
- Be silly. Change your background on Zoom to reflect mood or places you wish you could be, or use filters on your faces. This is one area where telehealth provides a whole new world of strategies that wouldn’t be possible in in-person sessions.
- Consider games that don’t require a screen share as well. Classics like “20 Questions” can be engagement-building hits with this population as well.
Transitional Age Youth (TAY)
For the TAY population, technology tends to already be their main mode of communication, connection, and entertainment. Telehealth now brings a needed service through a means they know and are comfortable with already. TAY have the option to not leave the comfort of their space to go to session with their service providers, which may lead to enhanced engagement and transparency. Many older teens have engaged in telehealth services with ease, due to already being tech-savvy and having frequent use of this means to connect with their peers.
There are barriers that exist with telehealth. For instance, for clients that struggle with isolation and depression, this may not be the best means for them as in-person contact and connection can better support with these challenges. However, with the incorporation of creative and interactive activities via telehealth, such as activities focused around integrated wellness or DBT activities, clients can still find support and help. Another barrier may be privacy. TAY tend to be serious about their confidential information being kept private and may shy away from participating if others, especially caregivers, are able to hear their sessions. Brainstorming options and solutions with the client at the start of treatment around confidentiality can be helpful.
Challenges to Consider and Potential Solutions
As mentioned above, confidentiality and privacy are very important to TAY. Trust can easily be broken, harming the therapeutic alliance, if not taken seriously and considered. Here are some ideas to talk with the youth about:
- See if earphones are available for youth to use
- Exploring if using telehealth outside of the home is an option to reduce risk of others overhearing
- Figuring out a time when less people are potentially present or are preoccupied with other tasks
- Incorporate more activities to express and communicate instead of traditional talk- therapy. For instance, journaling and sharing entries, “chatting” via telehealth, games, worksheets, etc.
If a client is unsure of telehealth, consider using the phone at first, and gradually shifting to a computer-based platform.
- First, have client join a telehealth platform with only audio. Next, have camera on but pointed at ceiling or a wall. Next, have an ear or an elbow in the frame. Gradually increase amount shown on camera and also length of time camera is on. Also normalize for client that you have anxiety/nerves about showing your face at times as well.
If a client exhibits psychosis or paranoia about virtual services, consider the following:
- Provide services on client’s desired medium of communication as well as different categories of comfort in medium e.g. telehealth can be audio only and no video or both audio and video
- Be creative. If you’re on your phone, you can take a walk while speaking to client (providing self-care to you as well as modeling this to client). You can encourage client to walk with you.
- Provide client at the beginning of treatment with psychoeducational material, coping skills worksheets, or worksheets for their specific diagnosis in order to have items of discussion in case client has nothing to talk about.
- Discuss with fellow colleagues or your supervisor interventions and resources available if not sure what to do next.
Rapport building is essential with any client, but could be more challenging with the TAY population. Preparing for this possibility will be essential.
- Be friendly and mindful of the energy level you bring, as youth may struggle with connecting if they don’t feel they can identify with your presentation
- Seek to understand their interests, hobbies, extracurricular activities, and peer relationships
- Be prepared with an age appropriate game or activity to engage youth if they are reluctant to talk
- Provide client with materials of discussion for the week, at the beginning of the week. (Send via email if client can print, or drop off material at their home if you’re able to capture case management time)
- Many of the intervention options listed in the previous section (Elementary and Middle-School Aged Population) can also apply with older youth as a means to increase comfort and engagement during sessions.
Assisting TAY with independent living skills can be much more challenging when you aren’t able to provide in-person support to engage a client in the community. This may require extra steps and thoughtfulness, but can be translated to the virtual world. Some strategies to consider:
- Think about what you can do virtually. For example, you may not be able to drive a client to a job interview, but you can help them complete their resume, engage them in a mock interview, or help them online shop for work appropriate attire. Note that you should always check with your supervisor about which of these types of activities are billable or allowable within your specific program.
- Engage clients in open discussion about barriers to their skill development. The absence of in-vivo intervening might provide opportunities for clients to bring increased insight to the nature of their challenge.
- Walk clients step-by-step through new skills. If a client is learning to ride public transportation (for example), share your screen and make a detailed list of all of the steps involved in this activity. Set goals around taking baby steps towards this larger goal and keep them accountable. Without in-person support, these types of goals may take longer to be achieved, but celebrate little steps along the way.
TAY tend to express themselves verbally with more ease than younger clients, which may increase the likelihood of a client sharing concerning thoughts, feelings, or behaviors with you. If your client is at risk of self-harm or suicide, expressing homicidal ideation, or is engaging in risky behaviors in the community (more global safety planning steps are discussed in detail in the “Addressing and Assessing Crisis Virtually” section of this toolkit):
- Obtain client location at the beginning of each session as well as any people near him or her
- Have the client identify location If using telehealth attempt to display a calm and relaxed manner
- Use active listening (Most times clients just want to feel heard)
- Apologize if interrupting client; this teaches appropriate social interaction
- Help client identify nearby resources, friends, or family members
- Create a safety plan with client if needed
- Provide client with different mediums of resources such as physical locations, phone numbers (VCSS after-hours line, Prevention line) and even mental health chat rooms (Takemyhand.co or Operation Safe House are great options to explore)
Group Work
There are many benefits to providing group-based services via telehealth. Groups of clients who previously may have been geographically challenging to bring together can now gather in one meeting. Groups can be easy to join from the comfort of clients’ own homes, which can encourage increased attendance. Additionally, clients can participate to their personal comfort level (such as having cameras off or participating only via the chat box initially).
Telehealth groups also require less coordination by facilitators to identify an appropriate location for a group session. Facilitators can host many groups in a day, even back to back, if there is a need to do so. They can more easily share video content during the group without relying on sometimes finicky technology systems at the usual group site.
Here are some primary considerations when providing a group via telehealth:
Co-Facilitators Recommended
Having a co-facilitator in the virtual room is helpful for many reasons.
- A co-facilitator can keep things flowing by helping respond to the chat, navigating technical issues, and responding to individual needs while the primary facilitator continues the session for everyone else.
- If a group member needs a break for de-escalation or one-on-one time, the co- facilitator and that group member can be put in a breakout room while the primary facilitator continues the session.
- Co-facilitators can provide the ability to respond to behaviors faster. For example, if something inappropriate is shared on the screen or in the chat, or there is distracting noise, it can be handled more promptly if someone other than the presenter has Zoom controls.
Confidentiality
Confidentiality considerations are particularly important to revisit frequently in group settings. You should set group agreements regarding confidentiality during the initial meeting, and swiftly and directly address any risks to confidentiality as they arise. Group members should be asked to:
- Join the group from a quiet, secluded space when possible, with nobody in the background
- Wear headphones
- Never take recordings or screenshots during session
- Not share details of the group or the other participants with anyone outside the group
Establishing Group Norms
In addition to discussing confidentiality agreements, you should also create group norms together during a first session; you will get more buy-in from participants when they take part in the process of establishing group norms. You can come prepared with some in mind to suggest and guide the participants in the right direction. Get specific with expectations for group members when they are calling in from home or another virtual location. Even if this discussion feels “obvious”, do not rely on shared assumptions of what is or is not appropriate. Some common agreements in telehealth groups might be:
- be dressed in appropriate clothing
- have a neutral background
- be in a quiet space with as little interruption as you can
- wear headphones
- mute when you’re not speaking
- take turns
- use the chat box feature to ask questions
- respond to prompts only
- use the “raise hand” feature when you want to contribute
Potential Barriers to Engagement
and Strategies to Troubleshoot:
Participants Don’t Want to Turn on Their Cameras
- Plan activities that may require the camera to convince participants to dabble with having it on. Consider activities with “show and tell” elements such as scavenger hunts or art projects. Sharing a personal object or their art as opposed to their face may be more comfortable for some at first too.
- “Require” the camera for only a small portion of the session. At the beginning of the session, tell participants which portions of the group will be most beneficial with cameras on or will require camera.
- Include those who have their cameras off by calling on them to answer questions, or reply to what they may share in the chat.
- Encourage participation in the chat box throughout the session. Adjust your expectations and allow for chat box participation to be considered meaningful and interactive.
Noisy Backgrounds are Creating Distraction for Facilitators or Participants
- Create a group norm that participants remain on mute when they are not sharing.
- Allow participants to use the chat box if they seem embarrassed or distracted when trying to talk through a noisy background.
- For large groups or groups with younger participants, explore the setting on Zoom in which participants can only unmute when the host invites them to do so.
- Utilize nonverbal communication when you want group participation but don’t want to open up to discussion for lack of time or when backgrounds are loud. Coach participants to stay on mute but provide thumbs up/down, ASL signs for yes/no, or use the chat box for voting. You can also teach participants how to use the “reactions” feature on Zoom.
Tech Issues such as Low Connectivity or Choppy Connection
- Before beginning the group, review steps for re-accessing the group if you lose connection.
- Have the co-facilitator help participants with specific technology problems in the chat box while you continue the group for the remaining participants.
- Keep phone numbers on hand for each participant so the co-facilitator can reach them via phone to help troubleshoot technology challenges.
Strategies to Increase Engagement and Participation from Group Members
- Know the names of each group member and call participants by name to encourage engagement and build relationship.
- Provide “choices” to increase ownership of the space. Allow group members to choose negotiable things such as background music, provide multiple options for activities, or host a vote for the following week’s activity.
- Play background music while working on anything written, such as journal prompts or worksheets. Utilize Zoom’s “share computer sound” function.
- Use interactive visuals. Google Slides is a great way to have visual and interactive games in which you can “move” things around on the screen.
- Educate yourself on online games that you can facilitate at low or no-cost. “Kahoot!” is a great example.
- Dedicate time to icebreakers at the beginning of each session. These can start groups off with a laugh, and are a low stakes way to get used to sharing.
- Look into websites like PollEverywhere to make interactive polls. Group members answer questions and these sites create graphs or word clouds that display group members’ answers live when you share your screen.
- Incorporate movement breaks, or games that require movement: chair yoga, stretch breaks, or scavenger hunts that require getting up and grabbing items. Consider encouraging group members to go for a walk together (note that you should consider safety precautions and seek guardian approval).
Helpful Zoom Settings and Tips Specific to Group Work
These are settings you can establish at the time you create the Zoom meeting. If you have a recurring group scheduled already and would like to change the settings, select the meeting and click “Edit”.
- Mute participants upon entry
- In “Chat Settings”: Choose if you’ll allow chatting to everyone or only the host(s). You can also choose whether or not group participants can send private chats to one another; it is recommended to turn this setting off to avoid distracting side conversations.
- Turn off participant screen sharing.
- Make your co-facilitator a co-host so they have access to all Zoom controls
Want More?
Watch these videos of a “mock” group created by the Victor team that detail strategies to employ when troubleshooting telehealth challenges:
- Group Introduction (18:32)
- Discussion on Ice Breakers (14:17)
- Discussion on Group Behaviors (14:52)
- Group Activity (13:45)
CFT Meetings
CFT Meetings are another service in which telehealth has opened doors for creativity and participation that extend beyond the limits that in-person services create. Formal and natural supports from anywhere in the world can now participate in CFTs more realistically, and scheduling or transportation challenges that may have previously prevented participation from group members can be side-stepped. Clients or their families may feel safer to participate in a virtual meeting, as it can feel less formal and intimidating. Many have found that virtual meetings are more “focused” and to the point, and less infused with conflict or emotion.
In the virtual “room,” the facilitator is tasked with holding and maintaining a space that invites active participation from all present. Many of the strategies and interventions described in the “Group Work” section of this toolkit apply to virtual CFT facilitation as well. However, the task of bringing together other professionals alongside clients and their families also presents some unique challenges in the virtual world. Some strategies specific to CFT facilitation are below:
Preparing for the Meeting
- List all Victor team members as meeting co-hosts in Zoom. This will be important if the facilitator or “host” is having technology issues on their end, is running late, or has to step away for any reason. Other team members are able to support and can minimize the time taken away from the meeting.
- Have the video call setup 10 minutes before the start of the meeting to ensure that all is functioning appropriately.
- Send email or text reminders to participants on the day of the meeting that includes the Zoom link and any relevant reminders.
- Ensure that clients and families are informed ahead of time about the structure of the meeting and who will be in attendance.
- Be sure that all participating team members are comfortable with the chosen platform and able to access it ahead of time. Some community partners request Victor’s Business Associate Agreement (BAA) with Zoom (which ensures encryption and confidentiality) prior to participation.
Keeping team members engaged and on track
- Greet all participants as they join and let them know when the meeting will start. Let participants know that full introductions will take place once the meeting begins.
- Create and adhere to Group Agreements (see page 22 for examples of agreements)
- Use an on-screen agenda. You can utilize PowerPoint or Google Slides to allow visual effects to pop in, which can increase engagement and visual stimulation.
- Use the “White Board” function in Zoom to take notes as you would during an in- person meeting.
- See the appendix for examples of PowerPoint slides that you can screen share to help guide the meeting.
- Consider whether or not you will request that all team members turn their cameras on. Some team members (youth in particular) may feel safer to participate more fully with their camera off.
- Call on specific team members for participation or contributions; some people will be less likely to speak up in a virtual setting than they would in-person. If you need specific information from someone or notice that someone has not contributed yet, ask for their input.
Follow-Up between Meetings
- Meeting Minutes can be typed by an additional team member during the meeting and dispersed to team members only minutes after the meeting ends. Having a team member act as the note taker also takes some pressure off of the Facilitator to multi- task.
- If any team members are struggling to participate virtually, someone from the team should connect with them between meetings to specifically discuss the virtual CFT process and troubleshoot identified barriers.
- Seek feedback proactively from team members about what is working and what can be improved on a regular basis.
Assessing and Addressing Crisis Virtually
One of the most anxiety-provoking elements of telehealth for many providers is the question of what will happen if a client is experiencing crisis. When a client becomes triggered and escalated during a session, or discloses suicidal intent, a lack of physical proximity can create barriers to maintaining immediate safety. However, appropriate pre- planning and swift, decisive action can be extremely effective remotely in dispelling crisis or preventing further harm.
First, have a clear understanding of the client you are serving. You already screen for potential safety risks during assessment.
Some of the risk factors that are contra-indicated for telehealth services are:
- Recent Suspected Child Abuse Reports
- Psychotic symptoms requiring in-person assessment
- Recent or current suicidal or homicidal ideation or recent attempts
- Recent crisis intervention services, inpatient psychiatric hospitalizations, or residential care step downs
- Clients who without treatment would be at risk for decompensation
If you are working with a client experiencing these risk factors, be sure you are in frequent communication with your supervisor about the most appropriate way to serve these clients to maintain safety; in-person support may be indicated. However, it can also be the case that these factors are new and emerging (previously unassessed), or that telehealth services are the only option available for serving a specific client.
Planning for Safety in an Ongoing Manner
West Coast Children’s Clinic provides a guide for managing ongoing suicidality via telehealth that is included in the appendix of this toolkit. While this guide speaks directly to suicidality as a risk factor, many of the components of the plan apply to other risk categories as well. As mentioned above, you will feel more equipped to manage crises as they arise if you pre-plan with all of your clients. When engaging in initial safety planning:
- Work with clients or their caregivers to identify an appropriate emergency contact and have this person’s information saved in your phone. This should be someone who can agree to remain in touch and nearby during your sessions, to respond quickly in-person if necessary. Ideally, this should be someone the client trusts.
- Be clear with your client about what types of statements and/or behaviors will prompt you to engage in further safety planning in the moment (it is ideal to have this discussion before these behaviors present themselves).
- Know who your back-up is as well. If there is a need to involve law enforcement or emergency services, understand ahead of time how you will do this without disengaging from the client. Strategies for this are listed in the next section.
- Always know the physical location of your client at the beginning of the session, in the event that additional support is required.
Responding to an Immediate Safety Risk
Despite our best intentions, sometimes situations arise in sessions that make it impossible to continue maintaining safety through virtual interventions only. In the event that this occurs:
- Remain calm and grounded. Validate what your client is experiencing and speak with them in clear directives.
- Do not get off the phone or computer with the client. Inform them that if connection is lost and you are unable to reach them again immediately, you will take additional steps of contacting their emergency contact or emergency services (as appropriate).
- Engage your back-up plan. You can do this via text if you are on the phone with the client already, or via phone if your session is taking place on the computer. If it feels inappropriate to multi-task in this manner, or if the client overhearing you would cause further escalation, it is recommended to reach out to your supervisor or another team member to help engage emergency response. Again, for clients at high risk of crisis, it is recommended to identify steps in this plan with your supervisor or teammates prior to a crisis occurring, to alleviate confusion in the moment.
- Be open with the client about the steps you’re taking, as much as is clinically appropriate. Calmly explain why you feel their safety is at risk and tell them about the steps you’re employing to get help to them.
- While waiting for help to arrive, continue to engage the client calmly. Remind them of their coping skills and continue to attempt to ground them. Mindfulness techniques that they can utilize with you to co-regulate are recommended (tell me what you see, tell me what you smell, tell me what you hear, etc.).
- Ensure appropriate follow-up with the in-person support when they arrive. This may require speaking directly to emergency services, or coaching the emergency contact in next steps. Do not disengage from the support until you feel confident that the immediate safety need has been managed.
- Take care of yourself. Managing crisis is always stressful, and managing crisis remotely can create new uncertainties that may be difficult to cope with. Ensure that you process the experience with your supervisor and explore what went well versus what you can learn for next time.
Wrapping It Up
We hope this toolkit has sparked your creativity and provided you with new strategies to utilize in your telehealth sessions.
While Victor's focus on telehealth as a service modality was generated largely by the onset of COVID-19, we expect that telehealth will continue to be a useful element of our global service delivery perspective even after pandemic restrictions lift.
Using virtual platforms to reach clients and their support people who might be otherwise emotionally or physically unavailable for participation in services holds true to our mission of being a catalyst for change.
Telehealth services allow us to do so with even more tools in our tool belt. We expect more innovations around telehealth care as we continue to learn and evolve in this area, and we encourage everyone to continue thinking outside the box for your clients, your program, and yourselves in this new adventure.
Appendix
Victor CQI: Telehealth Procedural Guidelines
Consent
- Obtain verbal or written consent from the patient for the use of Telehealth as an acceptable mode of delivering health care services
- Document in client chart that consent was obtained
The following topics should be discussed with client and guardian as part of the consent process and progress note should indicate the following:
- Inform the client that they have a right to confidentiality with Telehealth under the same laws that protect the confidentiality of their medical information for in-person psychotherapy.
- Inform client of their rights when receiving Telehealth treatment, including the right to stop or refuse treatment.
- Describe potential benefits (continuation of services being provided), constraints (internet or other technology issues), and risks such as privacy (session not taking place in a therapy room) and security of Telehealth (GoTo is encrypted and HIPAA compliant)
- Inform client of what will happen during the event of equipment failures during Telehealth sessions, and create a contingency plan.
Documentation
- All services should be documented in accordance with Medi-Cal standards
- Ensure your location code is identified in accordance with county direction
- Document in each progress note that Telehealth services were being provided due to "COVID-19 protocols"
Physical Safeguards
In order to remain HIPAA compliant and to maintain the integrity of your service, please be diligent of the following while providing Telehealth services.
- Only utilize Victor approved videoconferencing platforms
- Provider must be located in a private setting
- Encourage client to be in a private location
- Ensure no other client PHI is visible on the screen during a video session
- Utilize sounds machines when possible
- Present professionally as you would for an in person service
- Ensure laptops are kept on your person when in the community
- When storing agency issued electronic equipment and PHI offsite overnight, equipment and PHI should be brought into the home and when not in use, secured behind two locked doors, never left in a vehicle.
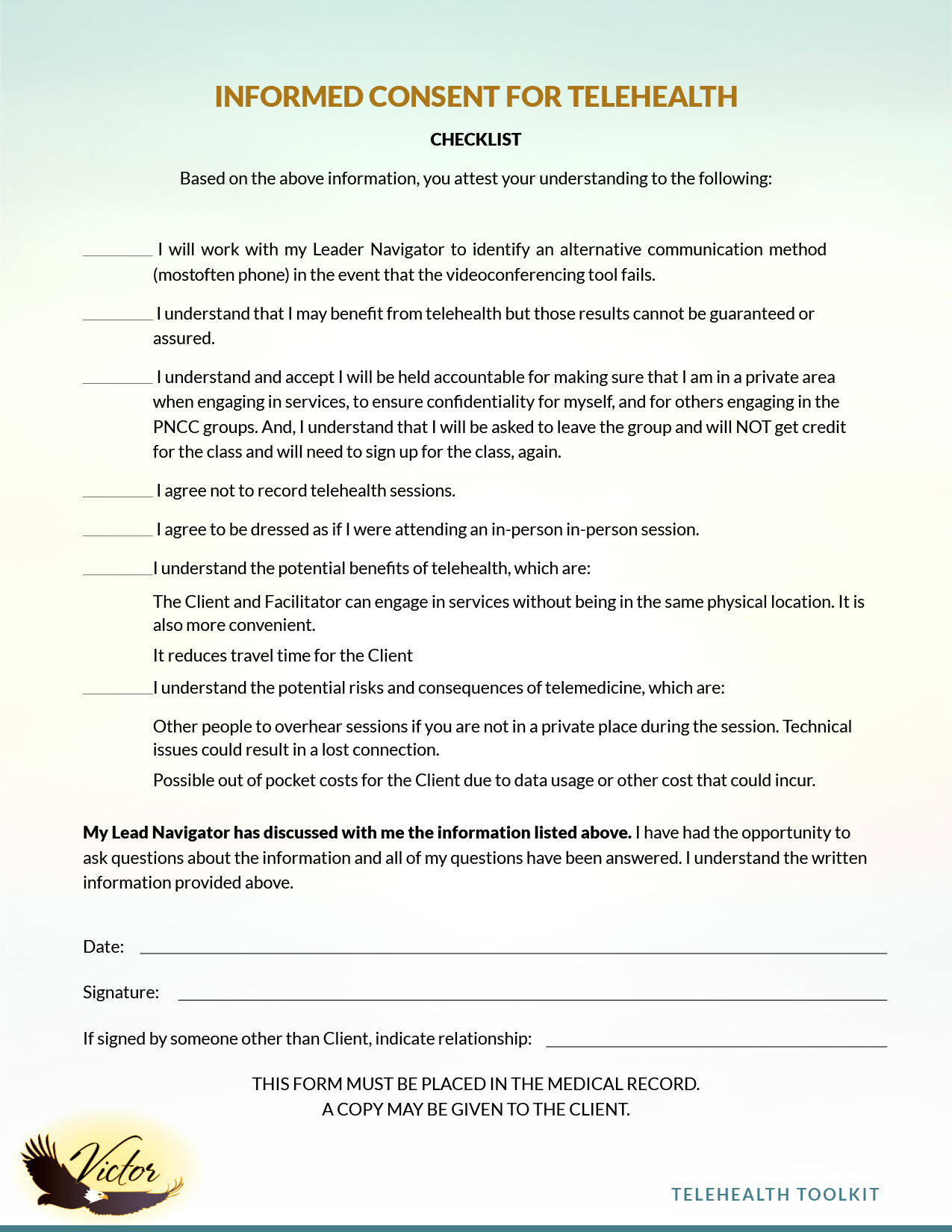
Informed Consent for Telehealth (example)
This Informed Consent for Telehealth contains important information focusing on providing healthcare services using the phone or the Internet. Please read this carefully, and let me know if you have any questions. When you sign or provide a verbal agreement to this document, it will represent an agreement between you and Victor Community Support Services.. You have the right to withdraw or withhold consent from telehealth services at any time.
Benefits and Risks of Telehealth:
Telehealth refers to providing services remotely using telecommunications technologies, such as video conferencing or telephone. One of the benefits of telehealth is that the Client and Facilitator can engage in services without being in the same physical location. This can be helpful particularly during the Coronavirus (COVID-19) pandemic in ensuring continuity of services. It is also more convenient.
Telehealth, however, requires technical competence on both our parts to be helpful. Although there are benefits of telehealth, there are some differences between in-person services and telehealth services, as well as some risks. For example:
- Risks to confidentiality. As telehealth sessions take place outside of your Facilitator or case manager's office at VCSS or the Probation Department, there is potential for other people to overhear sessions if you are not in a private place during the session. On our end, we will take reasonable steps to ensure your privacy. It is important; however, for you to make sure you find a private place for your sessions where you will not be interrupted. It is also important for you to protect the privacy of our session on your cell phone or other device. You should participate in services only while in a room or area where other people are not present and cannot overhear the conversation.
- Issues related to technology. There are many ways that technology issues might impact telehealth. For example, technology may stop working during a session, other people might be able to get access to our private conversation, or stored data could be accessed by unauthorized people or companies.
- Group Sessions: Each participant in the program will receive a consent form agreeing to the guidelines of group telehealth services, prior to the start of services, upon receiving and signing intake forms. However, we cannot ensure that each client will follow the guidelines. If it comes to the Facilitator's attention, during the session, that a client is not in a private area, the facilitator will ask the client to leave the meeting (or sign them out of the meeting), and will notify the Lead Navigator on client's case. This is to ensure that all participants, of the program, will have their information and what they share in the meeting kept confidential.
Electronic Communications
You may have to have certain computer or cell phone systems to use telehealth services. You are solely responsible for any cost to you to obtain any necessary equipment, accessories, or software to take part in telehealth.
Telehealth Needs Assessment
Created by West Coast Children's Clinic
Take a moment to identify where you can conduct telehealth sessions in your space. This could be a separate room, a multi-purpose room, a car, etc.
Understanding the restrictions of your space, choose what makes the most sense for you.
- What do you most like about your space?
- What do you most dislike about your space?
- What risks to confidentiality or privacy are present?
- What might be needed to better safeguard client information?
- How can you make your sessions as free from intrusions as possible? Are there ways to minimize potential distractions?
- What are some ways you might make your workspace feel distinct from your home?
- What routines or rituals might you try to maintain a work/life balance?
- What might you implement to give your sessions a consistent frame? Are there any routines or rituals you might use?
- Is it possible to plug into your ethernet (vs. relying on wi-fi)? Do you have sufficient space to charge your electronics in your space?
- How can you consider your ergonomic health in the space? For example, do you have an option to engage in some meetings from a standing position vs. sitting? Is your back well supported?
- What do you need in order to improve your space? Office supplies?
- Desk/working space supplies? Therapy supplies?
- What next step can you commit to do in the next week to address whatever needs have arisen as a result of this assessment?
Managing Suicidality
via Telehealth
Adaptations and Considerations
 PREPARE
PREPARE
- Request client location.
- Get emergency contact info.
- If needed, ask client if private space to talk is available.
- Who is your back-up? Work with a supervisor to practice a collaborative emergency rescue.
 ASSESS
ASSESS
- Use a screening tool (i.e., Columbia Suicide Severity Rating Scale/apps like SAFE-T) to assess risk and urgency of response.
- Re-visit safety plans, if they exist
- Assess the impact of the pandemic and changes in stressors.
- Assess for increased access to lethal means (e.g., medication stockpiles, weapons).
- Identify protective factors--reasons for living, deterrents. Have these factors have diminished recently?
 TAKING ACTION
TAKING ACTION
- Plans for more check-ins
- Consider alternatives to ER services, such as:
a. Crisis Support Hotline:
1-800-273-TALK
Text 'HOME' to 741741
b. Crisis Sessions with Community-based providers - Identify collaborators who can also monitor client's suicidal thoughts/behaviors. Ask to contact them.
- Develop a safety plan for clients to help manage suicide risk (e.g., safety plan worksheet, wellness-recovery-action-plan).
 STEPPING UP CARE
STEPPING UP CARE
- Call a team meeting
- Determine whether in-person sessions are clinically indicated
- Coordinate to determine how each team member will respond to the client, including in-person services.
- Managing acute crises is different from managing chronically severe MH needs. Telehealth may not always be the most clinically indicated service. Consider whether a higher level of care is needed.
 WHAT IF MY CLIENT'S
WHAT IF MY CLIENT'S
RISK IS IMMINENT?
- Some practices are the same:
a. Emergency Response Teams where available
b. 911
c. Going to the ER. - Stay online/on-phone as long as possible if there is someone arriving who will accompany your client to the ER.















 PREPARE
PREPARE ASSESS
ASSESS TAKING ACTION
TAKING ACTION STEPPING UP CARE
STEPPING UP CARE WHAT IF MY CLIENT'S
WHAT IF MY CLIENT'S